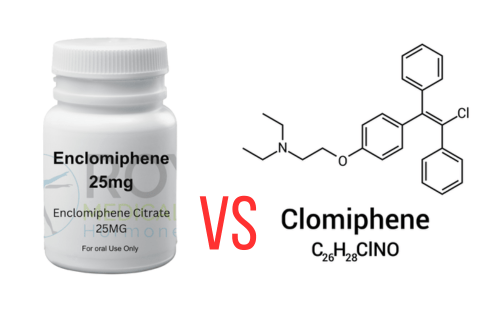
Clomid vs Enclomiphene
For men seeking testosterone therapy without traditional testosterone replacement therapy (TRT), Clomid (clomiphene citrate) and Enclomiphene are two SERM (Selective Estrogen Receptor Modulator) options. While both stimulate natural testosterone production, their differences in composition, side effects, and clinical outcomes are critical to understand. Below, we break down their key distinctions to help you make an informed choice.
Clomid (Clomiphene Citrate)
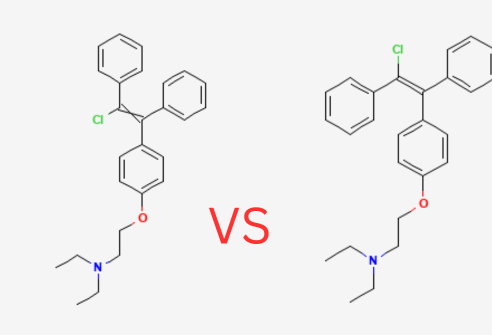
Clomid is a mixed-isomer SERM containing 62% Enclomiphene and 38% Zuclomiphene. Originally developed for female infertility, it’s used off-label for male hypogonadism. Clomid works by blocking estrogen receptors in the hypothalamus, disrupting the negative feedback loop and increasing LH and FSH production. This leads to higher testosterone levels. However, the presence of Zuclomiphene introduces estrogenic effects, potentially causing side effects like mood swings and vision changes. Despite these risks, Clomid remains a cost-effective option for testosterone therapy.
Enclomiphene
Enclomiphene is a purified form of the Enclomiphene isomer, developed specifically for men to optimize testosterone levels while minimizing estrogenic side effects. It acts as a potent estrogen receptor antagonist, disrupting the negative feedback loop to increase LH and FSH production, thereby boosting testosterone levels. Unlike Clomid, Enclomiphene avoids the mixed effects of Zuclomiphene, offering a more targeted approach with fewer side effects. Studies show it effectively raises testosterone without suppressing sperm production, making it a preferred choice for men who want to maintain fertility while addressing low testosterone.

Key Differences at a Glance
| Aspect | Clomid (Clomiphene Citrate) | Enclomiphene |
| Composition | – 62% enclomiphene (trans-isomer)- 38% zuclomiphene | – Pure enclomomiphene isomer |
| Mechanism of Action | – Blocks estrogen receptors- Mixed estrogenic/anti-estrogenic effects | – Selective estrogen receptor blockade- Avoids zuclomiphene effects |
| Testosterone Increase | – ~150–200 ng/dl rise- May fluctuate due to zuclomiphene | – ~150–200 ng/dl rise- More stable testosterone levels |
| Estradiol Impact | – Increases estradiol (+17.5 pg/ml in studies) | – Lowers estradiol (-5.92 pg/ml in studies) |
| Fertility Impact | – Zuclomiphene harms testicular health/sperm production | – Preserves semen parameters- Fertility-friendly |
| Side Effects | – Mood swings, vision changes, fatigue | – Headache, nausea (rare)- Better tolerated |
| Cost | – $30–$80/month (generic) | – $100–$300/month (compounded) |
| Availability | – FDA-approved for infertility- Widely available | – Not FDA-approved- Available via specialty clinics |
Side Effects
| Side Effect | Clomid | Enclomiphene |
| Mood swings | Common | Rare |
| Vision changes | 15% risk | <1% risk |
| Testicular shrinkage | Possible | No |
| Estrogen-related issues (e.g., gynecomastia) | Likely | Unlikely |
Who Should Choose Which?
Clomid May Be Better If:
- Cost is a primary concern.
- You tolerate zuclomiphene well.
- Fertility preservation isn’t a priority.
Enclomiphene Is Preferred If:
- Minimizing estrogenic side effects is critical.
- Fertility preservation matters (e.g., family planning).
- You’ve experienced Clomid-related mood/vision issues.
The Bottom Line
Clomid offers affordability and accessibility but carries higher side effect risks. Enclomiphene provides a targeted, fertility-friendly option with fewer estrogenic drawbacks, albeit at a higher cost. Work with a hormone specialist to determine which aligns with your health goals, budget, and tolerance for side effects. For personalized care and guidance, consider reaching out to Empower Men’s Health Clinic, where experienced specialists can help you decide if clomid or Enclomiphene is right for you.